A mild increase in SDMA reveals a patient’s greater risk of kidney disease and is often the earliest indicator
Key study takeaways
- After a single mildly increased SDMA, there was a 72% probability of a recurrent increase in SDMA within one year.
- 81% of animals with mildly increased SDMA that persisted had creatinine within the reference interval when SDMA was first increased.
- Half of cats and dogs had an increased creatinine by one year following a mild increase in SDMA that persisted.
- Increases in SDMA and creatinine warrant follow-up testing. Study data suggests follow-up testing within 1 month, as waiting longer may risk delayed diagnosis and/or disease progression.
Introduction
Identifying kidney impairment early and beginning proper therapy is known to extend patient survival.1,2,3 This highlights the importance of symmetric dimethylarginine (SDMA) as an early biomarker of glomerular filtration rate (GFR) that increases with as little as 25% loss of kidney function.4,5
Mildly increased SDMA concentrations (results in the 15–19 µg/dL range) make up 57% of the increased SDMA concentrations reported by IDEXX Reference Laboratories. Improved clarity is needed for the implications of a mildly increased SDMA concentration on the patient’s outcome. A mild increase in SDMA may be the first sign of a progressive decline in renal function, or it may be a signal of an acute event that will resolve. The clinical course and outcome of kidney disease in cats and dogs is often uncertain.
The purpose of this study is to provide a baseline expectation for the clinical course in patients that present with a mildly increased SDMA concentration, by assessing how often these results are persistent (followed by repeated instances of SDMA above the reference interval) and when creatinine is also increased. Additionally, it examines various follow-up timelines to recommend when to conduct further tests.
The International Renal Interest Society (IRIS) and IDEXX both provide information on how to stage kidney disease and what follow-up actions to take when renal disease is suspected.6,7 This study builds on these resources by examining the trends in renal markers for thousands of cats and dogs over the course of a year following their initial increase in SDMA, with particular emphasis on animals that presented with mildly increased SDMA results.
Study design
All U.S. cats’ and dogs’ chemistry panels submitted to IDEXX Reference Laboratories over a 22-month enrollment period beginning in July 2015 were considered for this study. Animals were required to be between the ages of 1 and 25 years old with at least 3 chemistry panels including the IDEXX SDMA Test performed during the enrollment period.
In order to limit inclusion of patients with ongoing renal impairment, the first result (T0) was required to be within the reference interval (RI) for SDMA and creatinine (SDMA ≤14 µg/dL and creatinine ≤2.3 mg/dL in cats and creatinine ≤1.5 mg/dL in dogs). The second result (T1) had no value restrictions. It was only required to follow a chemistry result that met T0 requirements. The third result (T2) was required to be between 14 days and 12 months after T1. This result and all subsequent chemistry results were used to assess the probability of future increased SDMA concentrations, concordance of creatinine, and to examine follow-up timelines. Of interest to the study were the 16,454 cats and 16,523 dogs for which T1 SDMA concentrations were above upper limit of the RI (14 µg/dL) and the comparison of their probability of an increased SDMA concentration on the next test to that of the 43,764 cats and 112,999 dogs for which T1 SDMA concentration was within the RI.
Methods
The probability of an increased SDMA concentration on the next test was calculated as the percent of T2 SDMA concentrations above the RI and were presented with 95% confidence intervals calculated using the binomial exact method. The Aalen-Johansen estimator for cumulative transition intensities was used to calculate the probability of creatinine results rising above the RI at any time after an increase in SDMA.8 Equivalence tests were used to compare persistence probabilities of cats and dogs with T1 SDMA concentrations of 15–19 µg/dL with follow-up testing within 1 month to those with follow-up between 1 and 6 months and those between 6 and 12 months. An equivalency threshold of ±5% probability of persistently increased SDMA concentration on follow-up (T2) was used at a significance level of 5% (P < .05) after adjusting for multiple comparisons using the Holm-Bonferroni method.
This study was limited by its reliance on retrospectively collected data, i.e., study cats and dogs had unknown diagnoses, treatments, and outcomes. Additionally, the study requirement that animals have 3 or more chemistry panels performed may have biased the sample towards animals that received more veterinary care or were in poorer health than the population that did not receive regular diagnostic testing. This study also may have been limited by survivor bias as animals that died before they could have 3 chemistry panels performed were not included. Study data did not include animals for which follow-up testing was not conducted for increased renal markers. The use of available test results means that timing between chemistry panels was variable, and potentially influenced by unknown confounding variables, and may not represent all follow-up activities.
Results
Figure 1 shows the probability of an increased SDMA concentration on T2 for each T1 SDMA concentration. In animals with T1 SDMA concentrations below the RI (≤14 µg/dL), the probability of an increased SDMA concentration on T2 was only 9%. The average probability for all animals with mildly increased SDMA concentration (15–19 µg/dL) was 48%, more than 5 times that of animals with a T1 SDMA concentration within the RI. Of the cats and dogs with mildly increased T1 SDMA concentrations that did not persist on T2, nearly half had an additional increased SDMA concentration within the year. This shows that following one mildly increased SDMA concentration, there is a 72% risk of further GFR impairment within 1 year (figure 2).
Figure 3 shows the percentage of increased creatinine in cats and dogs with persistently increased SDMA (T2 SDMA >14 µg/dL) for which the T1 SDMA concentration was mildly increased. At T1, only 19% of these animals had concurrently increased creatinine, increasing to 48% by 1 year.
T2 follow-up SDMA testing was conducted at various time intervals. To determine whether the timing of follow-up testing influences the probability that an SDMA concentration remains increased, this study compared the probability of persistence for mildly increased SDMA concentrations when cases are followed up within 1 month, between 1 and 6 months, and between 6 months and 1 year of initial increase. The persistence probabilities were equivalent to within ±5% (1–6 months: P < .001; 6–12 months: P < .001).
Probability of increased SDMA on follow-up by T1 SDMA concentration
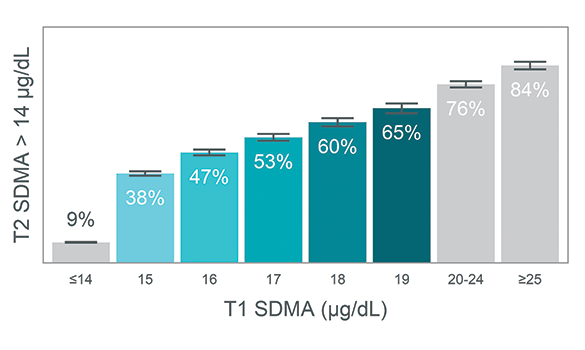
Figure 1. Probability of increased SDMA on follow-up increases proportionally with T1 SDMA concentration
Percent risk of increased SDMA concentration on follow-up testing following a mildly increased T1 SDMA concentration
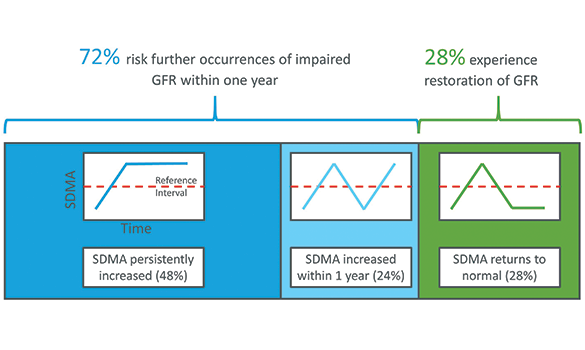
Figure 2. 72% of cats and dogs with a mildly increased SDMA concentration have another increased SDMA concentration within 1 year
Percent of patients with increased creatinine by time interval since persistent mildly elevated T1 SDMA concentration
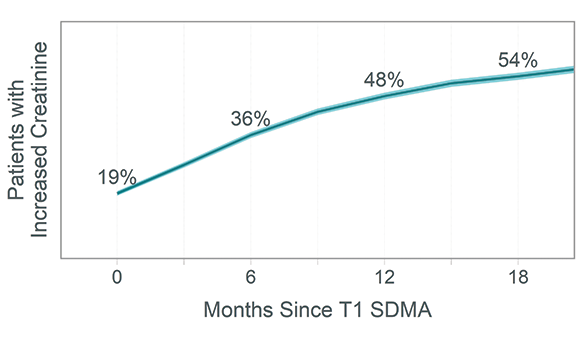
Figure 3. Mildly increased SDMA concentrations that persist often precede an increased creatinine
Discussion
This study demonstrates that mildly increased SDMA concentrations are most often the first indicator of impaired GFR and that they frequently persist. It also identifies the frequency, general time frame, and patterns of the progression of functional renal biomarkers. Notably, the probability of increased SDMA persisting rises appreciably through the mildly increased SDMA RI (15–19 µg/dL) and beyond. The 48% probability of continued GFR impairment on the next test represents a five-fold increase in risk over the population of patients that did not have an increased SDMA concentration on the prior test. Together, these points provide strong evidence for clinical investigation and follow-up of a single mildly increased SDMA concentration. The probabilities of persistence along the range of SDMA concentrations are similar to those of creatinine (IDEXX unpublished data),9 although an important difference is that a mildly increased SDMA concentration is the only indicator of decreased GFR 81% of the time in cases that persist.
Not all cases of impaired GFR are expected to persist, and potential reasons for restoration of SDMA concentrations back to within the RI include successful treatment10,11 (e.g., fluids, antibiotics, hypertension control, diet), renal compensation,11,12 repair from an acute event (e.g., dehydration, toxicity), early chronic kidney disease (SDMA concentrations at or near the RI),13 and biological or analytical variability. This study examined the risk of further GFR impairment in the population for which SDMA indicated restored GFR following an initial mildly increased SDMA concentration. In this study when mildly increased SDMA concentrations returned to within the RI and further testing was available from that year, 46% of patients had another increased SDMA. This suggests that a single increased SDMA indicates patients that have a much higher probability of future GFR impairment than the control population, even if this impairment appears to restore on follow-up testing.
The longitudinal examination of when patients with persistent mildly increased SDMA concentrations also developed increased creatinine demonstrates the sequence and timeline in which many patients experience progression of early kidney disease or continued GFR impairment. The data shows that increases in SDMA most frequently preceded increases in creatinine, and that by one year after an initial mildly increased SDMA concentration, nearly half of the cats and dogs also had increased creatinine. This evidence is highly supportive of prior reports that SDMA is a more sensitive and earlier indicator of reduced GFR than creatinine4,5,14 and provides an average timeline for serum renal indicators in a clinical setting beginning with mildly increased SDMA concentrations.
Follow-up testing can enable diagnosis of kidney disease or identify resolution of GFR impairment. Only 16% of mildly increased SDMA results in this study were followed up within 1 month, yet the probability of persistence is equivalent for all follow-up conducted within a year. Earlier testing could lead to earlier diagnosis prior to when creatinine also increases and may lead to more successful interventions.
Conclusion
This study shows the importance of recognizing and investigating a single mildly increased SDMA concentration. A mildly increased SDMA concentration with appropriate diagnostic follow-up can lead to the recognition of on-going impairment of GFR and the potential for kidney disease. These findings establish a timeline for progression and support a recommendation for follow-up diagnostics including the IDEXX SDMA Test within a month of initial increase. This study emphasizes that even with restoration of GFR, serial monitoring of SDMA and creatinine is warranted.
References
- Boyd LM, Langston C, Thompson K, Zivin K, Imanishi M. Survival in cats with naturally occurring chronic kidney disease (2000–2002). J Vet Intern Med. 2008;22(5):1111–1117. doi:10.1111/j.1939-1676.2008.0163.x
- Elliott J, Rawlings JM, Markwell PJ, Barber PJ. Survival of cats with naturally occurring chronic renal failure: effect of dietary management. J Small Anim Pract. 2000;41(6):235–242. doi:10.1111/j.1748-5827.2000. tb03932.x
- Jacob F, Polzin DJ, Osborne CA, et al. Clinical evaluation of dietary modification for treatment of spontaneous chronic renal failure in dogs. JAVMA. 2002;220(8):1163–1170. doi:10.2460/javma.2002.220.1163
- Nabity MB, Lees GE, Boggess MM, et al. Symmetric dimethylarginine assay validation, stability, and evaluation as a marker for early detection of chronic kidney disease in dogs. J Vet Intern Med. 2015;29(4):1036–1044. doi:10.1111/jvim.12835
- Hall JA, Yerramilli M, Obare E, Yerramilli M, Jewell DE. Comparison of serum concentrations of symmetric dimethylarginine and creatinine as kidney function biomarkers in cats with chronic kidney disease. J Vet Intern Med. 2014;28(6):1676–1683. doi:10.1111/jvim.12445
- IDEXX Laboratories. IDEXX SDMA algorithm. www.idexx.com/files/idexx-sdma-test-algorithm.pdf. Accessed March 26, 2020.
- International Renal Interest Society. IRIS staging of CKD (modified 2019). www.iris-kidney.com/pdf/IRIS_Staging_of_CKD_modified_2019.pdf. Accessed March 26, 2020.
- Odd A. Nonparametric inference in connection with multiple decrement models. Scand J Statist. 1976;3(1):15–27.
- Data on file at IDEXX Laboratories, Inc. Westbrook, Maine USA. (ID: 091_191231143138)
- Hall JA, MacLeay J, Yerramilli M, et al. Positive impact of nutritional interventions on serum symmetric dimethylarginine and creatinine concentrations in client-owned geriatric cats. PloS One. 2016;11(4):e0153654. doi:10.1371/journal.pone.0153654
- Dicker SE, Shirley DG. Mechanism of compensatory renal hypertrophy. J Physiol. 1971;219(3):507–523. doi:10.1113/jphysiol.1971.sp009675
- Hayslett JP. Functional adaptation to reduction in renal mass. Physiol Rev. 1979;59(1):137–164. doi:10.1152/physrev.1979.59.1.137
- Relford R, Robertson J, Clements C. Symmetric dimethylarginine: improving the diagnosis and staging of chronic kidney disease in small animals. Vet Clin North Am Small Anim Pract. 2016;46(6):941–960. doi:10.1016/j.cvsm.2016.06.010
- Hall JA, Yerramilli M, Obare E, Yerramilli M, Almes K, Jewell DE. Serum concentrations of symmetric dimethylarginine and creatinine in dogs with naturally occurring chronic kidney disease. J Vet Intern Med. 2016;30(3):794–802. doi:10.1111/jvim.13942